Microbial warfare
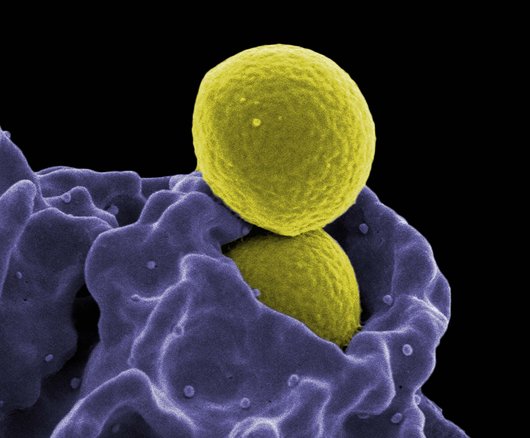
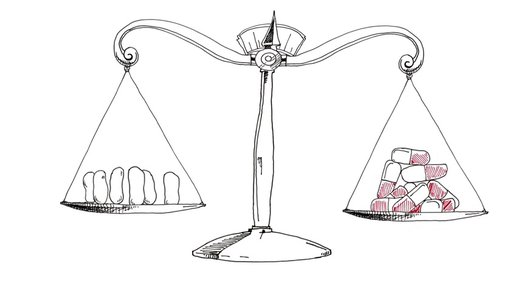
We mainly associate antibiotics with pills, yet these substances have a natural origin. All around us, as well as on the outside and inside of our own bodies, microbes are waging war on one another. Occasionally, they take up arms, in the form of antibiotics (from the Greek ‘anti’ (against) and ‘bios’ (life)). They use their defensive substances against competing bacteria, disrupting vital processes such as their growth, the construction of their cell walls, and the synthesis of proteins and genetic material. We use these very same substances in our own bodies, in the fight against pathogenic bacteria. Antibiotics are of no use against diseases that are caused by viruses, such as colds or flu.