Phagos
Viruses need a host to replicate. But a virus cannot use just any organism for this. They are extremely specific with respect to their target. Viruses that infect animals form a minority, and those that infect humans an even smaller subgroup of that minority. Most viruses actually target bacteria. For each of the millions of species of bacteria on Earth, there is a virus which specializes in infecting only that species. These are the so-called bacteriophages (-phage from the Greek phagos, which means ‘to eat’).
Cell hijackers
The underlying strategy of all viruses is pretty much the same. A virus attaches itself to recognition points on the cell membrane of its host and injects its own DNA into the cell. In this viral DNA lie the instructions for producing new virus particles. Once inside, the virus hijacks the native DNA-copy mechanism. While the host ‘thinks’ it’s processing its own DNA, it’s actually processing the viral DNA and producing new virus particles. These virus particles are then assembled into new viral units, called virions. After a while the host cell is completely full of virions and breaks open. This of course leads to the death of that cell.
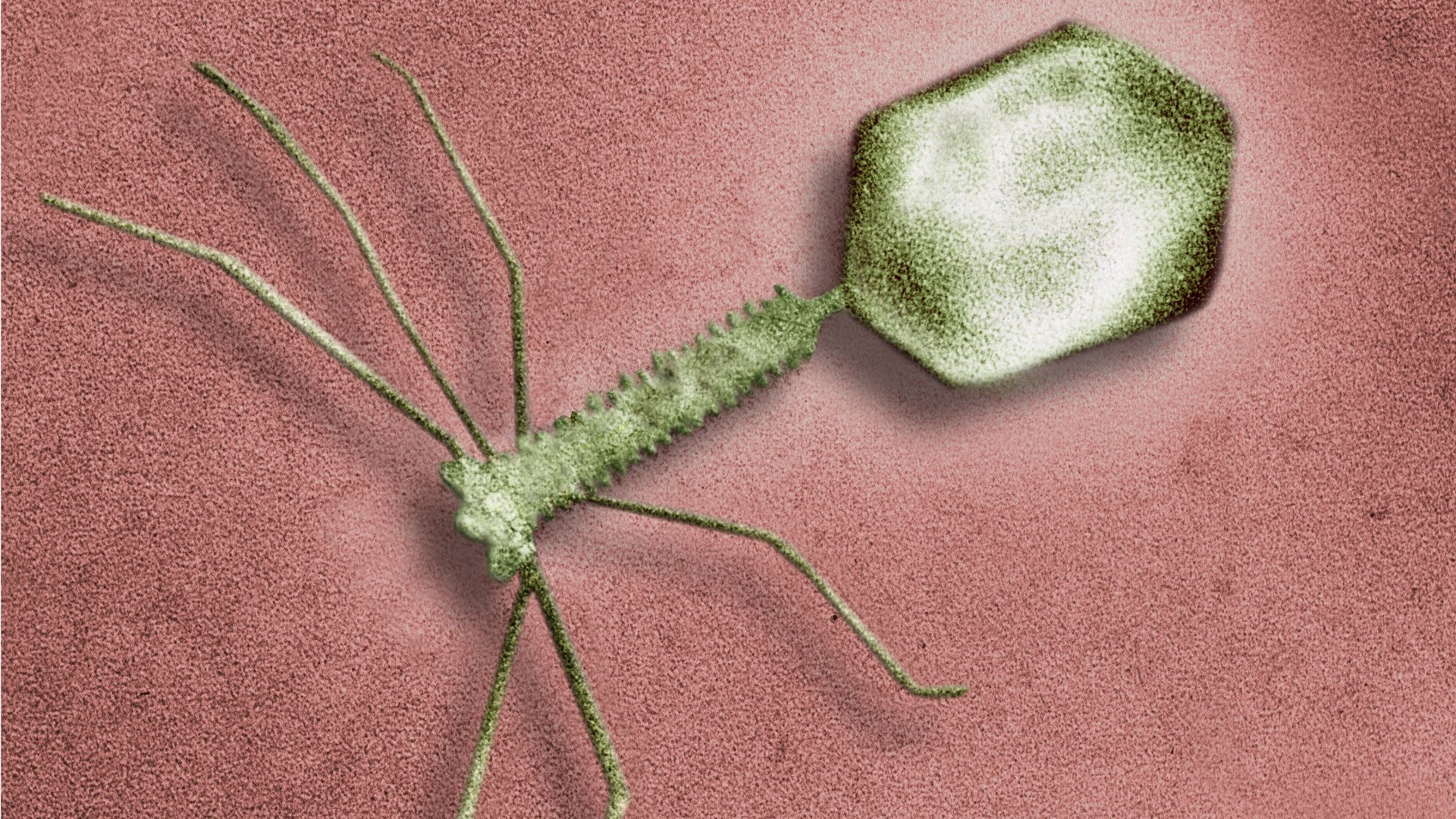
Bacterio phage
Long disregarded
With bacteriophages being so efficient and specific in their mode of action, it was a logical step to consider using them to treat bacterial infections. This is called phage therapy and it’s not a new concept. In fact, the antimicrobial action of bacteriophages was already proven 100 years ago. A lack of biological understanding of bacteriophages led to badly designed experiments, with poor results as a consequence. This, coupled with the simultaneous discovery of antibiotics which proved more effective and cheaper to produce, led to a standstill in phage therapy development. Only in the Soviet Union did interest remain and was this type of treatment in active use. Unfortunately the Cold War resulted in limited information exchange with the Western world, where the focus remained on antibiotics. However, with the emergence of antibiotic resistance it has become clear that antibiotics are not a sustainable solution and there is now renewed interest in phage therapy.
Many pros, few cons
One of the biggest disadvantages of antibiotics is that doctors are frequently required to prescribe a broad-spectrum antibiotic. This is because the exact cause of an infection is often unknown. As a result, not only the bacteria responsible for the infection are suppressed, but also a patient’s commensal microflora (the good bacteria). Bacteriophages on the other hand attack only the specific bacteria against which they are employed. This treatment also seems safe for the human body. Drug safety is measured in terms of the therapeutic index. The higher this value, the less likely side-effects are to occur, even when a drug is used in excess. Research has shown that the therapeutic index of phage therapy is higher than that of antibiotics. Also, only a few treatments are generally required to obtain a positive result because bacteriophages will multiply once administered. This is in contrast to antibiotics which are broken down in the body and need to be administered regularly over a longer period of time.
An obstacle to phage therapy lies in the diversity of bacteria. Within one species of bacteria there can be various strains. As mentioned, bacteriophages are extremely specific with respect to their target, often being strain-specific. Without knowing exactly which bacterial strain is involved in an infection it’s difficult to select the correct bacteriophage against it. To increase the chance of success, mixtures of closely related bacteriophages are frequently administered.

Escherichia T4 virus
Diverse applications
Considering the use of phage therapy in human medicine, the focus in the Western world has been mostly on the treatment of skin infections. Phage therapy has proven to increase the success rate of skin grafts where burn wounds were infected with antibiotic-resistant Pseudomonas aeruginosa. Treatment of Staphylococcus aureus infections in diabetic foot ulcers has also proven successful. Orally administered phage therapy for the treatment of Escherichia coli infections has been shown to resolve diarrhea. A recent publication told of an American patient who was in a coma for two months after becoming infected with antibiotic-resistant Acinetobacter baumanii, subsequently waking and recovering fully just two days after administration of phage therapy. But there are also numerous applications beyond human medicine, for example in agriculture (crop protection) and in environmental sanitation (wastewater treatment).
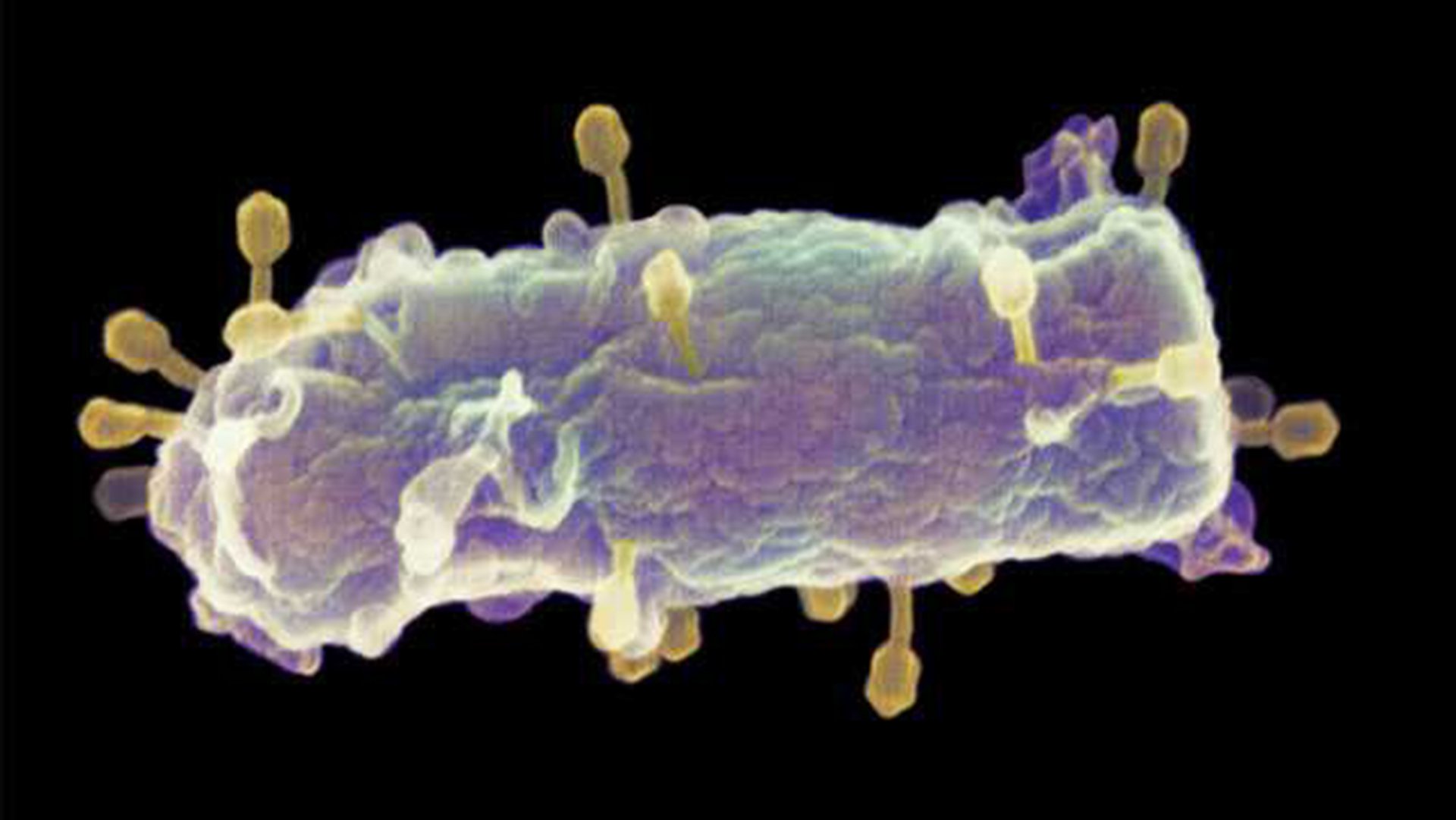
E. coli bacteria with phages (in yellow) on the cel wall.
Future?
Currently large-scale bacteriophage use is limited to the food industry where products have been developed to prevent Listeria, Salmonella, Shigella, and E. coli contamination during food processing. Human treatment with bacteriophages has yet to be approved in Europe or the United States. The biggest hurdle is a lack of knowledge about the safety of phage therapy. However, research to that end has intensified given the many benefits that phage therapy offers, and the results seem very promising for the future.
