Imbalance
The intestinal microbes in our digestive system are not only important for digestion, but also for our immune system and nervous system function. Unfortunately, interventions such as antibiotics have a negative impact on the composition of this so-called intestinal microbiota. Antibiotics do not only enter the bloodstream but also the intestines, where they kill benign bacteria and cause an imbalance. Such an imbalance can lead to various health problems. Sometimes antibiotics are prescribed in combination with probiotics. However, these probiotics are often also susceptible to the antibiotics and cannot replace the lost intestinal microbiota.
Cheese bacteria
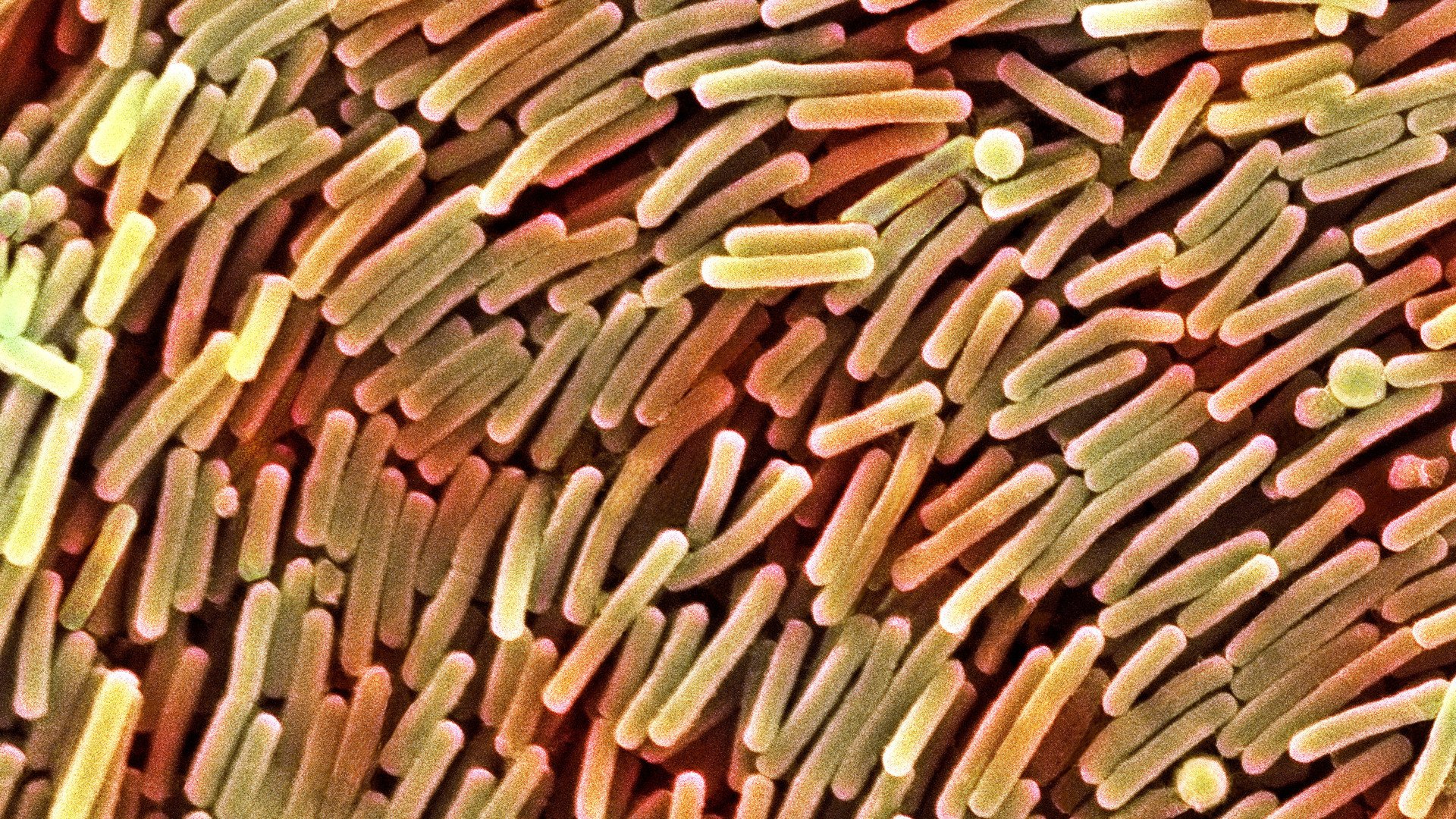
MIT researchers therefore engineered a bacterium that protects the intestinal microbiota. They gave the bacterium Lactococcus lactis, which is normally used to make cheese, the property of making the enzyme β-lactamase in the intestines. This enzyme breaks down the β-lactam antibiotics that reach the intestinal tract. These antibiotics, such as ampicillin and amoxicillin, make up about 60% of the antibiotics prescribed in western societies.

Lactococcus lactis
Effective
To test their idea, the researchers gave one group of mice two oral doses of the bacteria for each injection of ampicillin. Another group of mice was only given the antibiotics. The modified bacteria found their way into the gut and began to produce β-lactamase. In these mice, the researchers found that the amount of ampicillin circulating in the bloodstream was just as high as in mice that did not receive the bacteria. Moreover, the microbial diversity in their intestines remained much higher.
Also, none of the mice given the bacteria developed opportunistic intestinal infections (C. difficile), whereas all mice given only antibiotics had many C. difficile bacteria in their intestines. The researchers also discovered many genes for antibiotic resistance in the gut microbes in mice that received only antibiotics. These genes can be passed on to other (harmful) bacteria, thus exacerbating the problem of antibiotic resistance. And after their work was completed, the modified bacteria were neatly excreted again.
Clostridium difficile
Risks covered
However, the use of modified bacteria that break down antibiotics comes with risks. The production of the β-lactamase is a form of antibiotic resistance. Bacteria can easily spread their genes among each other - a process called conjugation or horizontal gene transfer. In theory, this could also happen to the genes encoding for the β-lactamase enzyme, which would make pathogenic species insensitive to these antibiotics as well.
To avoid this problem, the researchers changed the way the bacteria make the enzyme. They broke the gene for β-lactamase into two parts. By putting both parts elsewhere in the genome of the bacterium, it is very unlikely that both parts will be shared with another bacterium via horizontal gene transfer.

